
The medical student had to relay the tragic news to her family; “this newborn child does not have a mother because she got an infection.” This whole experience left our student baffled with questions surrounding the quality of breathing tubes. After identifying the breathing tube as the problem, he realized that someone needed to make a better breathing tube. Such a device would need to prevent fluid, bacteria, viruses, and other pathogens from reaching the lungs, but more importantly, it would need someone to devote themselves to creating it. “And I said, ‘I’m going to make a breathing tube that will prevent cases like this from ever happening again.'”
His name is Benjamin Wang, MD, and we are pleased to say that he honored his pledge. Today, Dr. Wang founded NeVap, a company producing breathing tubes that have been instrumental in saving the lives of COVID-19 patients. Our Top Doctor Magazine team was delighted to learn about Dr. Wang’s work and its role in the pandemic.
We employed Dr. Wang’s knowledge to write a thorough article on how an overlooked detail is becoming critical in caring for the sickest patients during the pandemic. Let us learn how Dr. Wang’s approach could be the turning point in the battle against ventilator-associated pneumonia and COVID-19!

Ventilator Systems and VAP
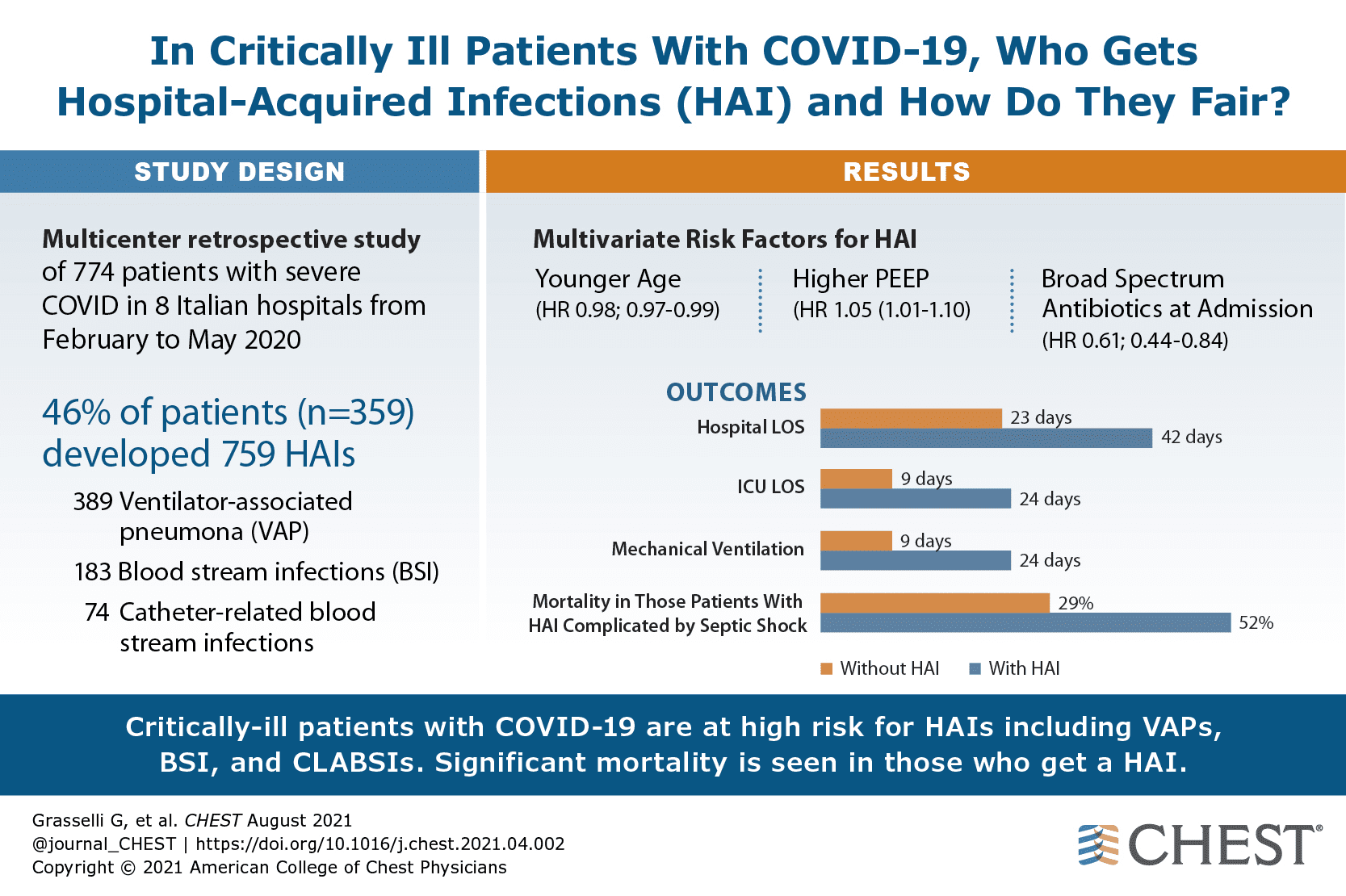
Although frequently critical, invasive mechanical ventilation is not devoid of risks. Because of the invasive nature of endotracheal or tracheostomy tubes, oropharynx or stomach secretions, rich with bacteria, will almost always leak along with the airway device into the patient’s lungs. The longer a patient spends on a ventilator, the higher their risk. The inability to protect the patient’s lower respiratory tract leads to numerous cases of VAP and unnecessary fatalities amongst COVID-19 patients (44%-50% rate of VAP in COVID-19 patients).
The Introduction of Single Port Subglottic Suctioning
Ventilator systems were improved by creating breathing tubes that could drain secretions before entering a patient’s lungs. Over the past 15 years, single port subglottic (i.e., under the tongue) suctioning endotracheal and tracheostomy tubes have been clinically beneficial by reducing VAP incidence (40%-67%), antibiotic exposure, length of mechanical ventilation, and mortality. Compared with previous technology, subglottic suctioning is a clear step forward.
However, this new technology is not without flaws. For example, respiratory care practitioners must often deal with subglottic suction blockage due to entrapment of airway tissue, often exceeding 50% within 5-15 minutes. In addition, due to both the device’s efficacy and reduced clinical benefits, only approximately 20% of hospitals currently utilize this class of breathing tube. Consequently, using these tubes effectively in Operative or Emergency settings hasn’t been possible, further limiting the number of patients who can benefit from these devices.
Multiport Subglottic Suctioning
To improve the safety of mechanical ventilation, Dr. Wang and his NeVap team set about creating a solution that could improve the efficacy of subglottic suction drainage in the ICU and bring this technology into other settings to benefit patients who would otherwise not be helped. They determined that a breathing tube that could reduce aspiration in all settings without engaging airway tissue could benefit clinicians and patients without requiring any additional equipment. Thus, the NeVap Aspire
Subglottic Suction Endotracheal Tube, or ASSET, was born after several years of development.
The ASSET tube uses 24 suction fenestrations and a tissue blocker to significantly reduce suction blockage while providing more effective suction removal of the secretions that cause VAP. The tissue helps point suctioning away from the patient’s tissue and decreases the distance between the suction source and airway fluid. In testing, NeVap ASSET removes ten to fifteen times more secretions responsible for VAP when compared to other tubes. It has been successfully used in a variety of patients during surgical procedures and emergencies.
A Superior Way of Preventing VAP
Dr. Wang and his team have devoted nearly a decade to develop what he believes to be the most logical and straightforward way to prevent VAP. Aside from superior design, NeVap ASSET is already benefiting patients in ways no other breathing tube has been able. Patients who need transplant surgeries, cardiac surgeries, trauma patients, and even COVID-19 patients benefit from better infection prevention due to the NEVAP breathing tube. In addition, this simple device benefits patients without using any chemical or pharmacological agents, so its infection prevention benefits can be used indefinitely. Moreover, with the average VAP treatment costing hospitals over $40,000/case, the NeVap ASSET is a clinically significant innovation and a critical way to save hospitals.





0 Comments